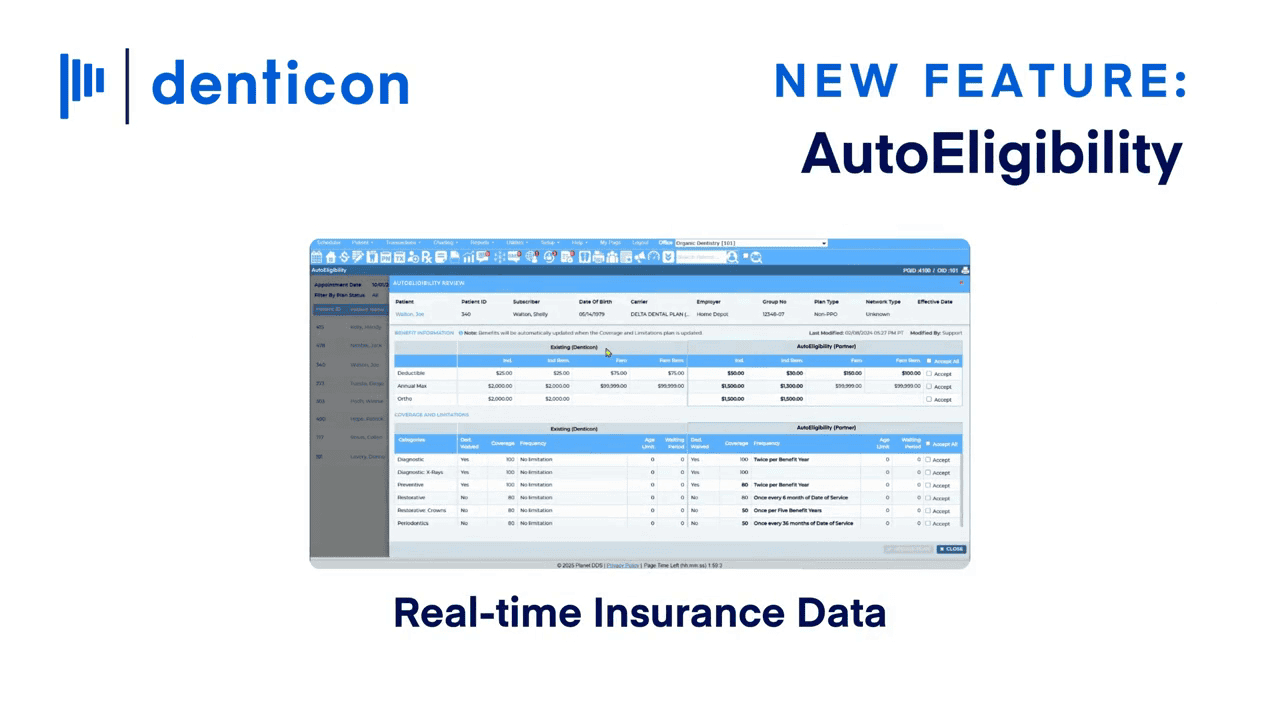
AutoEligibility – Fewer denials. Faster collections. Stronger cash flow.
AutoEligibility eliminates portal logins and payer calls by surfacing standardized eligibility and coverage details. This includes deductibles, frequency limits, and Medicaid directly inside Denticon.
- Speed up collection — fewer rejections, faster collections.
- Prevent denials before they happen — cleaner claims.
- Save 4-6 hours of work for the front desk each day.
- Improve patient trust — accurate estimates, no surprises.
Prevent Denials Before They Happen
"*" indicates required fields
Prevent Denials Before They Happen
Automate Eligibility Check inside Denticon
Prevent Denials
Detailed coverage data (not just “yes/no”) helps staff avoid rejections. Fewer write-offs, fewer billing errors, and faster cash flow.
Stronger Cash Flow
AutoEligibility prevents errors at the source — improving first-pass yield and speeding up collections.
Improve Patient Trust
Patients get accurate cost estimates that lead to higher satisfaction, fewer billing disputes, and stronger case acceptance.
Learn More About AutoEligibility
No portals. No phone calls. Just real-time answers in Denticon.